The robot has a high-tech camera on one arm and a high-tech sewing machine on a second arm. It’s already reattached halves of a pig’s intestines.
“It’s like park-assist in a car,” said Axel Krieger, an assistant professor of mechanical engineering in Hopkins’ Whiting School of Engineering. “Performs the procedure autonomously.”
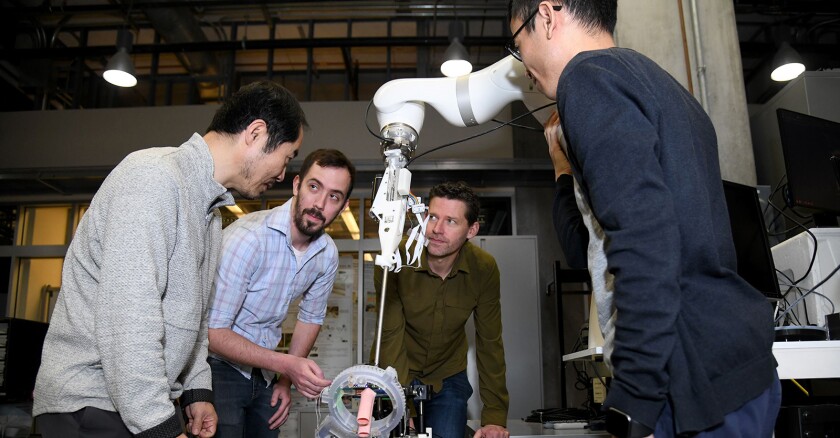
This kind of suturing is performed more than a million times a year in surgeries around the country, said Krieger, part of a team developing the robot and senior author on a recent paper describing the technology in Science Robotics.
The goal is to develop in the next several years a robot that makes the intricate and delicate work of suturing more consistent. Missing a stitch or doing one awkwardly could cause a catastrophic complication for a patient. The robotic procedure is also less invasive as it’s performed laparoscopically, through small holes in the skin rather than a large opening.
The Hopkins engineers expect the robot to be cheaper than existing robotic technology and more portable. They want to develop a mobile version that eventually could be used on an ambulance or in the field for emergencies, such as stitching up a major artery to stop bleeding.
The robot would advance technology currently in wide use in operating rooms. The U.S. Food and Drug Administration calls them robotically assisted surgical devices.
The best known is the da Vinci robot federally approved for general laparoscopic surgical use in 2000. The device has a console where a surgeon can see a 3D image and move several arms with surgical instruments, essentially becoming an extension of the doctor.
“The device is not actually a robot because it cannot perform surgery without direct human control,” the FDA says.
The da Vinci robot is now commonly used in gallbladder removal, hysterectomies and prostate removals because it works best on “complex tasks in confined areas,” according to the FDA.
Other robotic machines assisted in surgery before da Vinci was developed but required far larger incisions.
The new robot being developed by Hopkins engineers along with collaborators at the Children’s National Hospital in Washington, D.C., known as Smart Tissue Autonomous Robot, or STAR, is different. It does have computer monitors that offer a 3D view, but it doesn’t have a joystick or other controls.
The STAR is run by a highly advanced, and adaptable-on-the-fly computer program. The algorithm “sees” and “feels” through cameras that create 3D images with lasers and sensors that detect pressure from breathing, bleeding and soft tissue.
The robot completes about a stitch a minute, a conservative pace slightly slower than a human surgeon. The tests so far have shown more consistency than the humans.
That’s been an issue with robotic technology now in the operating rooms. The current robotic-assisted technology is better at some surgical tasks than others. And outcomes aren’t always an improvement even if things appear to go smoothly.
Such machines also add significantly to the expense of surgery because the cost of the equipment reaches into the millions, though some of that can be made up through shorter hospital stays and fewer complications. But many smaller hospitals and those in less affluent regions or other countries can’t afford upfront expenditure.
Jin Kang, another STAR developer and a professor in the Hopkins department of electrical and computer engineering, said the STAR requires less machinery and would be cheaper, though the ultimate cost is not determined.
It was designed with input from surgeons, who often choose to use technology because it can help them withstand the rigors of their job. Long hours of traditional surgery can cause human hands to twitch and fatigue.
He said surgeons and other surgical staff still would perform procedures, such as removing diseased tissue, before handing off to STAR, and would stay in the room in case of an emergency as the robot reconnected intestines or other vessels.
“Doctors are not being replaced,” Kang said.
Dr. Michael Awad, the director of the Barnes-Jewish Hospital Comprehensive Robotics Program in St. Louis, was not involved in STAR’s development but has been following the work at Hopkins. He did his surgical residency at Johns Hopkins Hospital and trained on the first generation of da Vinci robot there.
Awad said it’s still early in the process, but he believes autonomous robots are inevitable in the operating room and the Hopkins researchers work could be a big step forward.
How long it take the public — and surgeons — to accept such technology remains to be seen, he said.
He views it like those autonomous cars. People are ready to adopt the park-assist technology Krieger referenced and other technology to keep people from drifting into other lanes. The fully self-driving cars will prove trustworthy eventually, as well.
“While driving is high stakes and can result in injury or death, I think people are even more sheepish when it comes to surgery on the human body,” he said. “There are a lot more variables that make the task more challenging in itself. There is a higher bar to leap.”
Awad, who is also director at the Washington University Institute for Surgical Education, said there is a lot of training that goes into using existing robotic equipment. Doctors have to learn to use other senses such as their eyes on computer screens, rather than the touch of human tissue, when they use technology.
He said the machines are especially helpful in getting to tight and sensitive spots in the body such as the esophagus, behind the rib cage and near the heart. An autonomous robot could advance what doctors are able to do for patients.
There also may be less training needed for autonomous robots in the operating room. But that doesn’t mean surgeons won’t have to know how to perform the same procedures, Awad said.
“If a human needs to intervene, they need to know how to,” he said. “But anything that can lessen the learning curve would be welcomed.”
A position paper from the American College of Surgeons says surgeons need to be “appropriately educated and their skills assessed” prior to using any new technology. The group also calls for evaluation to establish the value and safety of the technology before wide adoption.
The Hopkins team plans to continue perfecting the robot and assessing what it could do beyond connecting two ends of a blood vessel, an intestine or other channels, called anastomosis.
Work on the robot has been supported by the National Institute of Biomedical Imaging and Bioengineering. A next step is seeking a commercial partner to bring the technology through the development process and approvals from federal regulators to begin testing the robot on humans.
“We really want to push the boundaries,” Krieger said.
©2022 The Baltimore Sun. Distributed by Tribune Content Agency, LLC.